Illustrated Inflammation & Pathology of Acne | Acne Development Illustrations
Light Acne © 2015 Galderma. Illustrated by Laura Maaske
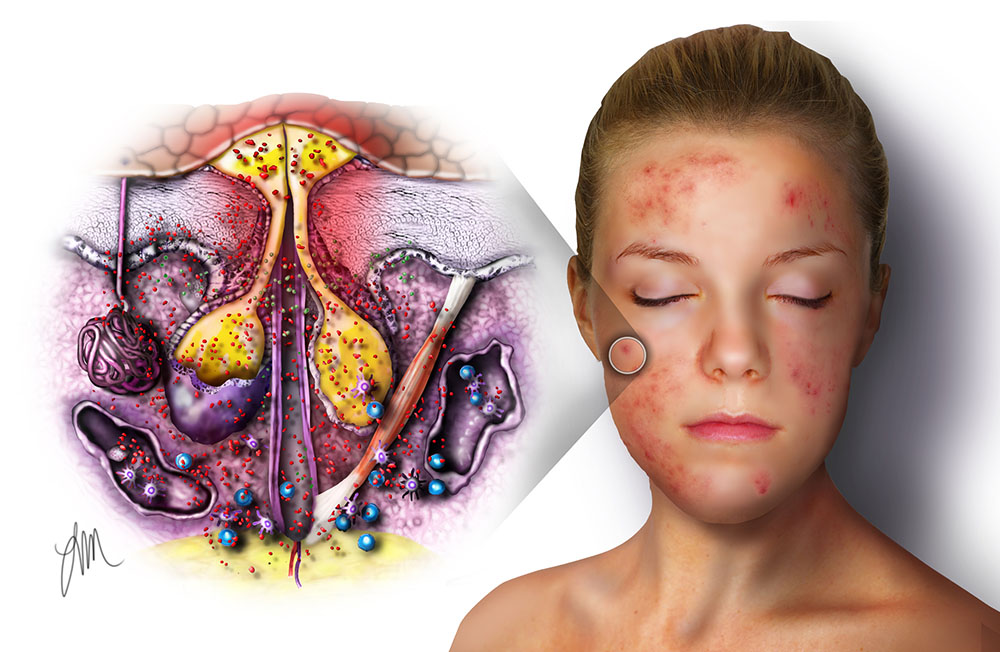
Acne Illustrations
Written and illustrated by Laura Maaske, MSc.BMC, Medical Illustrator & Medical Animator
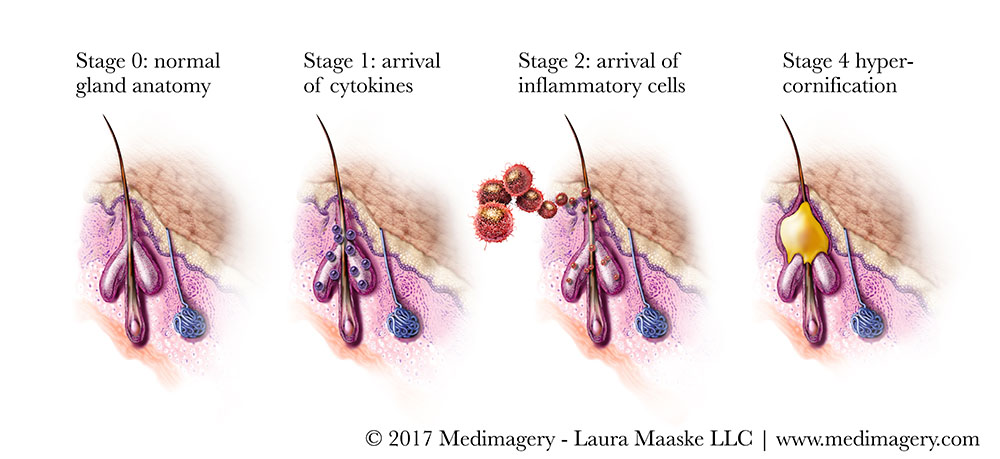
Development of acne
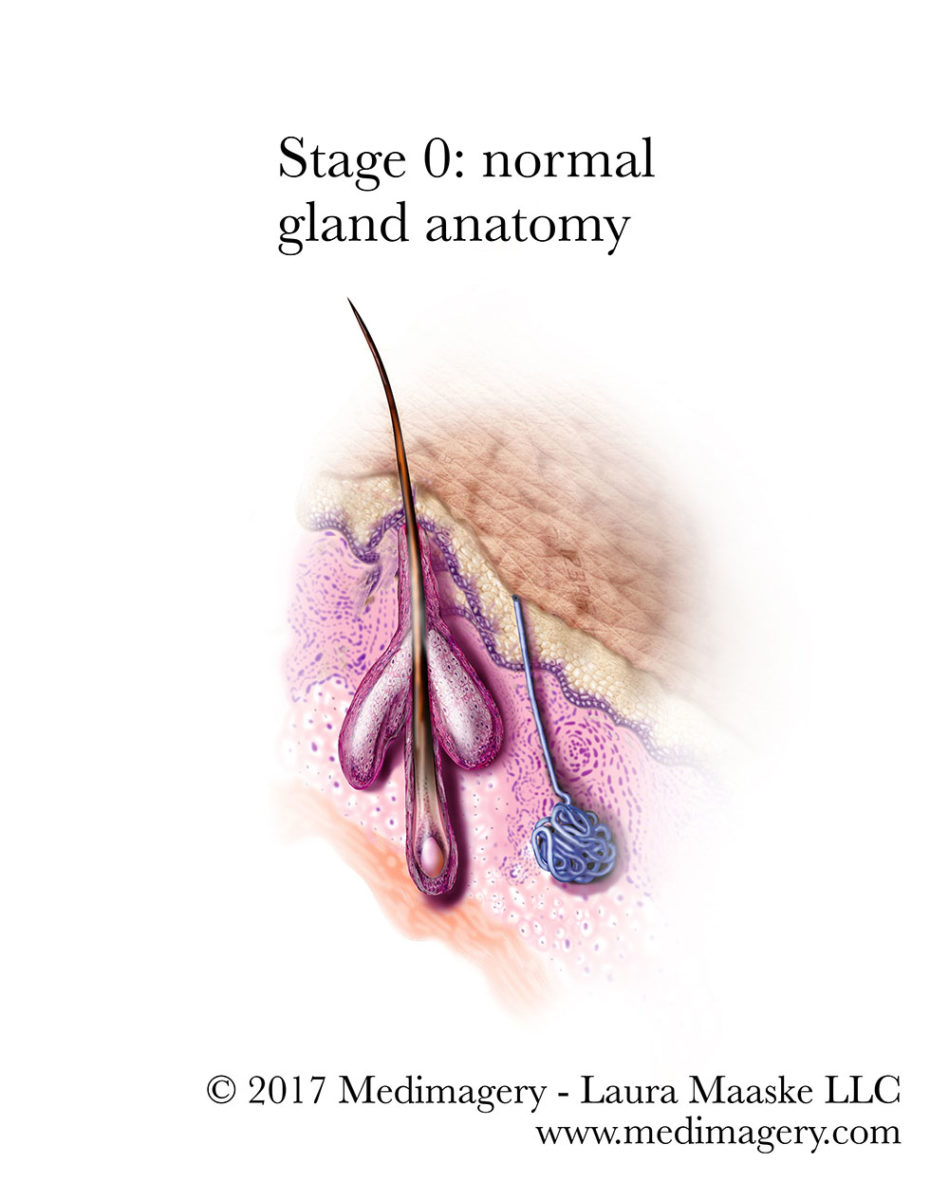
Stage 0: normal gland anatomy
Stage 1: Arrival of Cytokines
Propionibacterium acnes, is an anaerobic bacteria commonly associated with acne. Over 100 years ago, the presence of propionibacterium acnes (also known as P. acnes) was identified histologically (by examining a microscope slide) as present in acne. It was seen present at the sebaceous gland beginning somewhere by the end of its first day and its third day of development. In fact, clinicians were able to create new acne in unaffected patients by introducing propionibacterium acnes directly into the sebaceous gland. Despite this experiment, it is normal for all people to have this bacteria on their skin. Not everyone develops acne. And so, the presence ofpropionibacterium acnes is not a direct cause of acne.
Propionibacterium acnes isn’t the only bacteria associated with acne vulgaris. Staphylococcus, streptococcus, and candida albicans area all associated with acne, as well, to a less direct degree. Like Propionibacterium acnes, they infect the sebaceous glands in the same regions of the body: cheek, forehead, chin, and back.
While it has long been understood that the immune response is involved in acne at later stages, increasing histological and immunological evidence found from observation reveals inflammation fundamental process throughout the development of acne lesions, beginning even as the acne lesion is only 6 to 72 hours old. For more about this, refer to this article by Dr. Emil A Tanghetti. Researchers looking under the microscope found histological evidence for a buildup of lymphatic fluid (liquid swelling) at the site of an acne lesion.
While the causal and exact mechanisms are still not well understood, inflammation seems to occur at this very early in the development of acne lesions (microcomedones), even before the swelling is evident. In fact, when the clear and unaffected skin from acne patients was examined, it was found to contain high levels of CD3+ and CD4+ T cells, as well as a high level of macrophage at the site of yet-unaffected sebaceous glands.
It is now thought that propionibacterium acnes triggers inflammatory cytokine responses in acne by activation of TLR2. TLR2 is a protein found in the surface membrane surrounding cells. It is a receptor which recognizes foreign materials and microorganisms, and which sends signals on to immune cells in response to foreign materials. This triggers various cytokines and chemokines that stimulate recruitment of a larger immune defense response and involvement of immune response genes.
As a result of this understanding, TLR2 has become a target for researchers in the search for effective acne treatments. If drugs or treatments can prevent TLR2, the subsequent immune response and development of pustules may be averted. Cytokines are inflammatory substances produced by monocytes in response to invading gram-positive organisms.
P. acnes has been shown to trigger various players in the immune response:
- Pro-inflammatory cytokine release
- Expression of antimicrobial peptides (compounds made up of two or more amino acids linked in a special way, in a carboxyl chain group)
- Activation of monocyte TLR2. TLR2 in turn triggers the production of IL-12, IL-8, and ?-defensin-2.
?-defensins are a family of antimicrobial peptides produced in the skin in response to microbial infection. They elicit changes in cell migration and maturation, further release of cytokines, and serve to attract a further array of immune cells.
To further complicate the mechanisms, fatty acids found within sebum may contribute to TLR responses, either to increase or decrease the immune response.
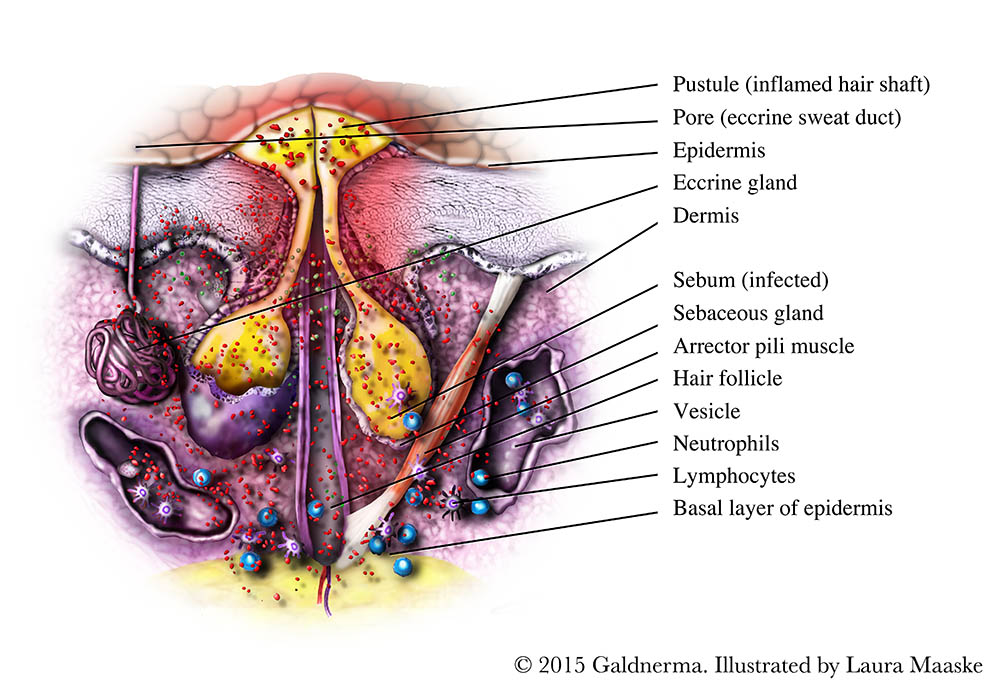
Stage 2: the arrival of the inflammatory cells
A combination of increased sebum production and abnormal hyperproliferation of keratinocytes results in the formation of a small microscopic lesion called a microcomedo. Subsequent accumulation of sebum, enlargement of the follicle, and build-up of keratinous material within the microcomedo cause the formation of comedones.
As the new lesion ages, polymorphonuclear leukocytes collect at the acnes lesion site, leading to greater swelling (distention) and pustule formation.
Stage 3: Hypercornification
Obstruction of the pilosebaceous canal precedes the development of the bumpy appearance associated with acne. The obstruction may be mediated be androgens and is produced by the accumulation of adherent keratin and excess sebum within the duct of the pilosebaceous unit. The duct also contains bacteria and saprophytic yeasts (yeasts that live on dead or decomposing matter). In turn this leads to expulsion of corneocytes (uppermost skin layer). This enlargement of acne pustules is also known as hypercornification. The process of hypercornification dilates the follicle, distorting its shape in all directions. The hyperkeratinization leads to either closed comedones (whiteheads) or open comedones (blackheads). Hypercornification may lead to rupture of the pilosebaceous follicle wall.
Treatments for acne
Adolescents and adults who deal with acne suffer from embarrassment and sometimes skin scars. Treatments for acne have improved slowly over the years. Despite popular beliefs, there are no links associated with cleanliness, sunlight, or cigarette smoking with acne.
There are essentially 4 different approaches for reducing acne.
- Reduce the inflammatory response at the site of acne
- Attack the P. acnes itself
- Adjust bodily hormone levels to combat androgens in the area
- Reduce sebum and skin shedding so the sebaceous canals remain open and unblocked
- Some new evidence suggests that a low sugar diet might improve acne
1. Reduce the inflammatory response
Anti-inflammatory Agents
Benzoyl peroxide (BPO)
Benzoyl peroxide (BPO), applied as a cream, kills P. acnes by oxidizing proteins within the bacterium. Benzoyl peroxide is also mildly effective at breaking down comedones and reducing inflammation. What makes BPO a strong recommendation is that it hasn’t been shown to increase bacterial antibiotic resistance.
Retinoids
Retinoids have anti-inflammatory properties, reduce sebum production, modify the sebaceous follice pore in ways which allow the release of sebum.
Retinols are related to Vitamin A . They come in several forms, and can be applied as crams, which include adapalene, isotretinoin, retinol, tazarotene, and tretinoin.
Azelaic acid
Azelaic acid is anti-inflammatory and antibacterial. For mild or moderate acne cases it can reduce acne when applied to the skin as a cream, twice a day for six months.
Salicylic acid
Salicylic acid has several impacts. It is anti-bacterial, it is karatolytic, and it opens up the pores of the sebaceous glands to allow the release of sebum and dead skin cells.
2. Attack the P. acnes itself
Antibiotics
Traditionally a standby in treatments of acne, antibiotics are incrasingly out of favor due to antibiotic resistances which are developing, as well as due to the ill effects on the digestive system function. Specifically, there is an increasing amount of antibiotic-resistant P. acnes worldwide, especially topically applied antibiotics such as macrolides and erythromycin.
Topical antibiotics are typically recommended for the less severe inidence of acne, and oral antibiotics for the more severe cases. Effective antibiotics, taken either topically or orally, may include metronidazole, clindamycin, sulfacetamide, and tetracyclines such as doxycycline and minocycline.
3. Reduce androgens
In teenage girls and women, androgens are produced by the ovaries. Taking a birth control pill reduces the androgen levels in the body, which reduces sebum levels in the sebaceous glands.
Antiandrogens such spironolactone, (not approved by he FDA) and cyproterone acetate may be used for women who are known to have high androgen levels or excessive sebum.
Hormonal therapies in general are not safe for women planning to become pregnant, or lactating. The hormone adjustments interfere with the development of the embryo and fetus.
4. Reduce sebum and skin shedding so the sebaceous canals remain open and unblocked
Nicotinamide is an anti-infammatory agent and reduces sebum production.
5. Low sugar diet
Some new research is pointing to sugar as a trigger in the body’s inflammatory response cycle. By reducing sugar in the diet, acne itself may be reduced.
Less interventive approaches to preventative acne care
I was hesitant to include everyday advice for those who suffer from acne. I stumbled upon a lot of old world advice and alternative treatments in my search for useful and reliable advice. However, in my personal experience, the findings of NIH are the most reliable tooks. And so, I am offering that advice here:
How Should People With Acne Care for Their Skin?
Clean Skin Gently
If you have acne, you should gently wash your face with a mild cleanser, once in the morning and once in the evening, as well as after heavy exercise. Wash your face from under the jaw to the hairline and be sure to thoroughly rinse your skin.
Ask your doctor or another health professional for advice on the best type of cleanser to use.
Using strong soaps or rough scrub pads is not helpful and can actually make the problem worse. Astringents are not recommended unless the skin is very oily, and then they should be used only on oily spots.
It is also important to shampoo your hair regularly. If you have oily hair, you may want to wash it every day.
Avoid Frequent Handling of the Skin
Avoid rubbing and touching skin lesions. Squeezing, pinching or picking blemishes can lead to the development of scars or dark blotches.
Shave Carefully
Test both electric and safety razors to see which is more comfortable. When using a safety razor, make sure the blade is sharp and soften the hair thoroughly with soap and water before applying shaving cream. Shave gently and only when necessary to reduce the risk of nicking blemishes.
Avoid a Sunburn or Suntan
Many of the medicines used to treat acne can make you more prone to sunburn. A sunburn that reddens the skin or suntan that darkens the skin may make blemishes less visible and make the skin feel drier. However, these benefits are only temporary, and there are known risks of excessive sun exposure, such as more rapid skin aging and a risk of developing skin cancer.
Choose Cosmetics Carefully
While undergoing acne treatment, you may need to change some of the cosmetics you use. All cosmetics and hair-care products should be oil free. Choose products labeled noncomedogenic (meaning they don’t promote the formation of closed pores). In some people, however, even these products may make acne worse.
For the first few weeks of treatment, applying foundation evenly may be difficult because the skin may be red or scaly, particularly with the use of topical tretinoin or benzoyl peroxide.
Direct Source: https://www.niams.nih.gov/health_info/acne/#acne_k
The larger perspective
Stage 1: the cytokines
Stage 2: the arrival of the inflammatory cells
Stage 3: hypercornification
February 28, 2017
Laura Maaske, MSc.BMC, Medical Illustrator & Medical Animator
e-Textbook Designer | biomedical communicator | Medical Visualizer